When the heart skips a beat (Literally!)
A 90-year-old gentleman rolls into ED with chest pain. Now, right off the bat, a 90-year-old with chest pain always gets your attention, especially with a history of hypertension.
You're thinking about all the usual suspects, right? But then the monitor catches your eye. His heart rate is chillingly low, just 35 beats per minute! GCS is still 15, thankfully, and the rest of his vitals are looking pretty stable, but that bradycardia is screaming for an answer.
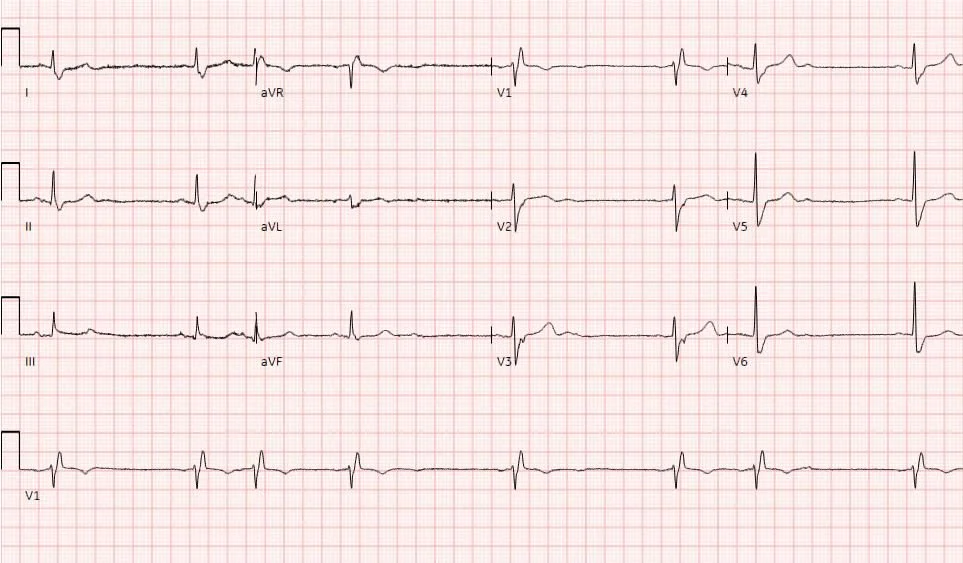
So, we slap on the ECG leads, and what do we see? This beauty right here:
This is Mobitz Type II Second-Degree AV Block. Not the friendly Wenckebach that often comes from AV nodal issues; this one's usually infra-nodal and a bit more sinister. Those dropped beats happen without a progressive PR prolongation, and they're often a sign of trouble brewing further down in the conduction system.
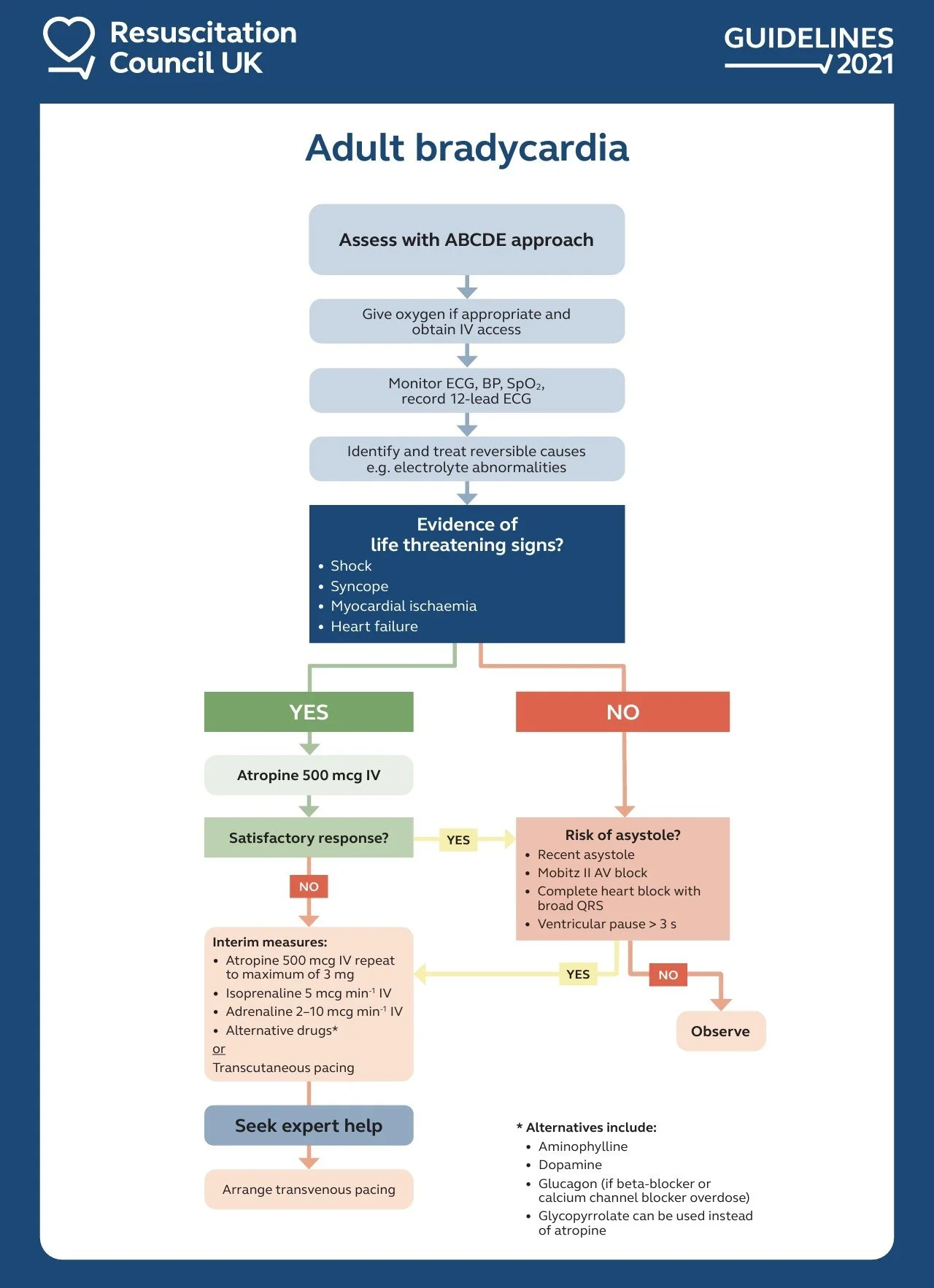
Given his chest pain and that super slow heart rate, we couldn't just sit around. He was symptomatic from that bradycardia. So, we reached for the atropine. And just like that, his heart rate started to climb, and he felt better!.
Bradycardia ResusUK
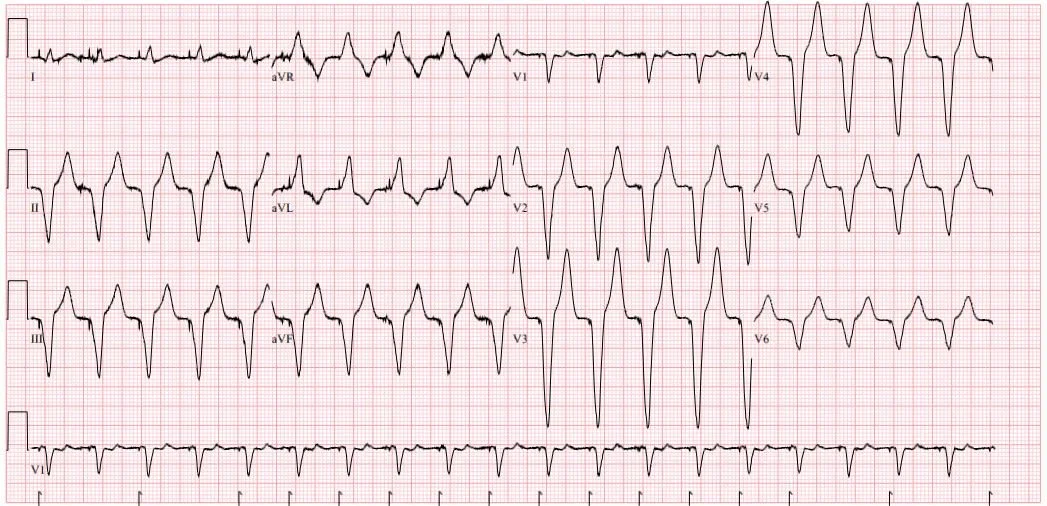
a Mobitz Type II in a symptomatic patient often points towards a need for something more definitive. And indeed, a few days later, after stabilization and further assessment, our 90-year-old received a dual-chamber pacemaker.